Medicaid Changes in 2023: How to Keep and Engage Your Members
By Ravisankar CJ on Tue, Apr 11, 2023

Medicaid faces significant changes in 2023 that could significantly impact Medicaid Members and Managed Care Organizations (MCOs). The expiration of the Public Health Emergency occurring later in 2023 sets up changes to Medicaid enrollment, impacting and changing the coverage of millions of Americans.
MCOs will play a critical role in helping their members learn about these changes and how to help them transition through them successfully. To best prepare your organization, learn what these changes are, how they impact your members, and what you can do to help them below.
How Medicaid is Changing in 2023
The sweeping changes to Medicaid introduced at the start of the COVID-19 pandemic are ending. The Public Health Emergency from the pandemic is expiring in 2023. This emergency power temporarily allowed for an easing in enrollment standards for members to help them maintain their coverage during an unprecedented and uncertain time.
As part of the expiration of the emergency powers, and as approved in the Consolidated Appropriations Act, continuous Medicaid member enrollment will end. Instead, the process used before the pandemic will resume, and individuals seeking coverage must re-enroll yearly. Additionally, Medicaid members will need to take action to complete their enrollment process rather than counting on their automatic enrollment.
How These Changes Impact Your Members
For those currently enrolled in Medicaid, these changes could result in a loss of coverage if they fail to renew coverage or meet eligibility requirements. The Kaiser Family Foundation estimates that up to 15 million people could lose Medicaid coverage during this process, of whom about 6.8 million are potentially eligible.
Why would those who are potentially eligible fail to receive coverage? The most common reasons are that they are unaware of these changes or don’t know how to complete the re-enrollment process. This is where MCOs will play a critical role.
How Your Organization Should Respond
It’s critical for your MCO to be proactive with your Medicaid members as these changes take effect.
First, aim to best inform your members about the upcoming changes and how they could impact their Medicaid coverage. Use digital outreach methods, such as reminder texts and phone calls, to remind members of upcoming renewal deadlines and changes to their benefits. FCC has guided that health plans can use text and automated calls to assist members with redetermination.
Second, consider offering additional information to your members about your marketplace plans for continuity of coverage should they become ineligible. The more information you can provide your members, the better.
Conclusion
Changes to the Medicaid program will significantly impact millions of people who rely on it for coverage. MCOs and other stakeholders must proactively engage with members, educate them on these changes, and guide them through the redetermination process. To leverage a software solution that can help you achieve this efficiently, see how HealConnect can help.
You May Also Like
These Related Stories

Agile Methodology of Software Development - Pros and Cons
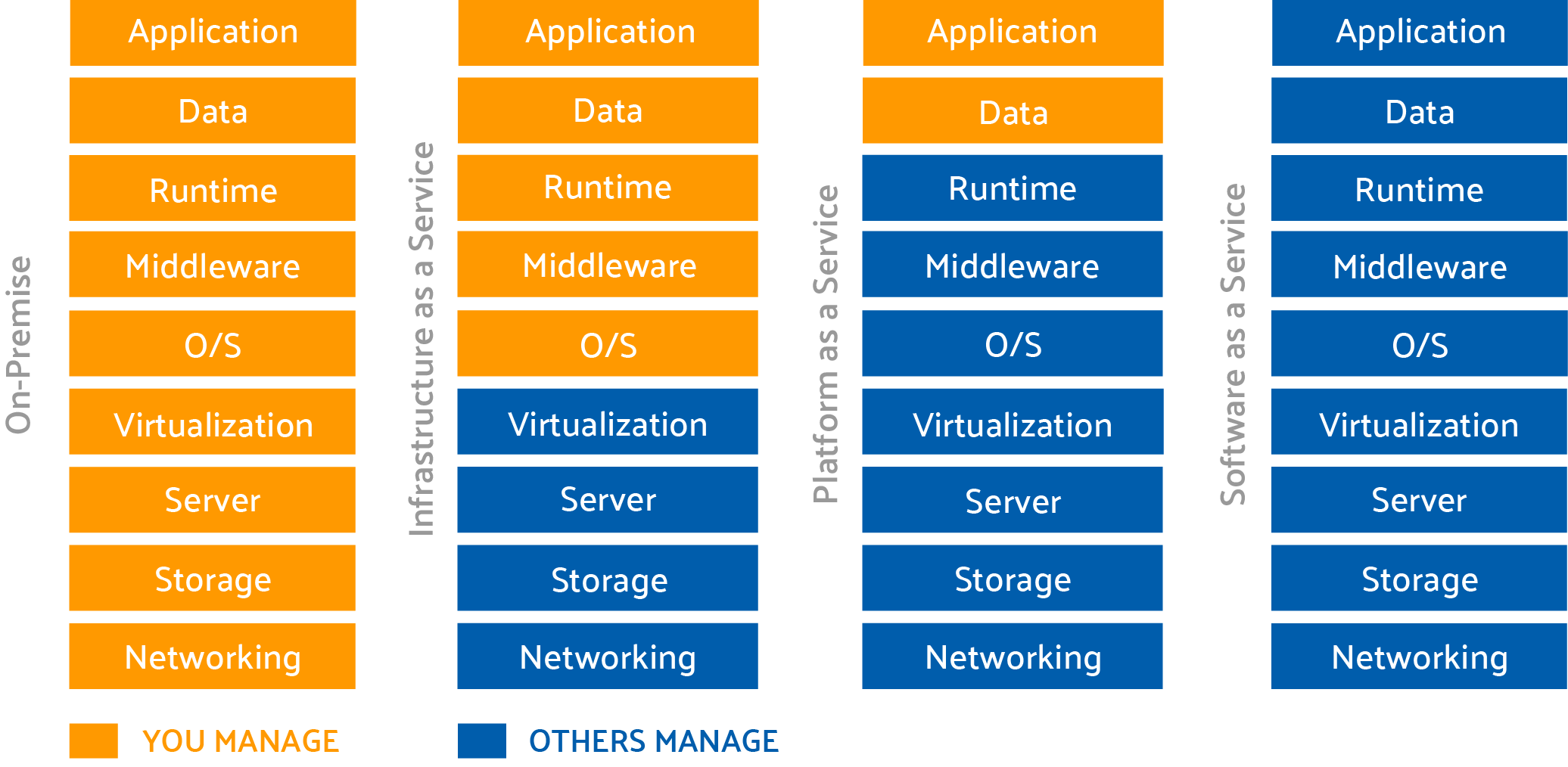
Moving to the Cloud? Here are Some Questions to Consider.



No Comments Yet
Let us know what you think