How Payers Can Prepare for Payer to Payer Data Exchange
By Lakshminarayanan Saravanan on Tue, Mar 09, 2021

Getting ready for payer-to-payer data exchange as part of the CMS Interoperability mandate? If so, your priority as a payer is to address the need to aggregate your members' data from various former payers. While this mandate focuses on empowering members, it also makes payers rethink how member data needs to be aggregated and distributed.
During the initial member enrollment, the requesting payer needs to obtain members' consent to retrieve their claims/encounters and clinical data from the former payers. The requesting payer must setup and validate system interactions with other payers as a prerequisite before any data exchange can happen. More importantly, payers need to create a plan for maintaining and expanding their list of data exchanges as more organizations are requested by members over time.
Requesting payers have two options to meet the payer to payer data exchange mandate:
- Option one: Expect your vendor's solution to have a payer endpoint registry that continually gets updated.
- Option two: Choose a vendor solution that leverages a directory service managed by an industry consortium entity, like CAQH, which contains tested, validated, and continuously enhanced payer endpoints.
Either approach will help payers meet the upcoming compliance deadline, but the second option offers greater efficiencies and potentially lower costs over time. Vendors and payers will need to work to get their interactions tested and validated with other payers.
Sagitec's HealFHIR solution, a managed FHIR infrastructure hosted in a HITRUST certified environment, adopts the CAQH directory service for its payer endpoint lookup service. Sagitec's HealFHIR solution has been tested, validated, and published as part of CAQH's beta program. The managed services infrastructure has an operationalized payer provisioning process that has been integrated with the CAQH payer's FHIR endpoint registration process. This ensures that if new payer endpoints are added to the CAQH directory, HealFHIR will integrate with those new payers by testing and validating the data exchange interfaces.
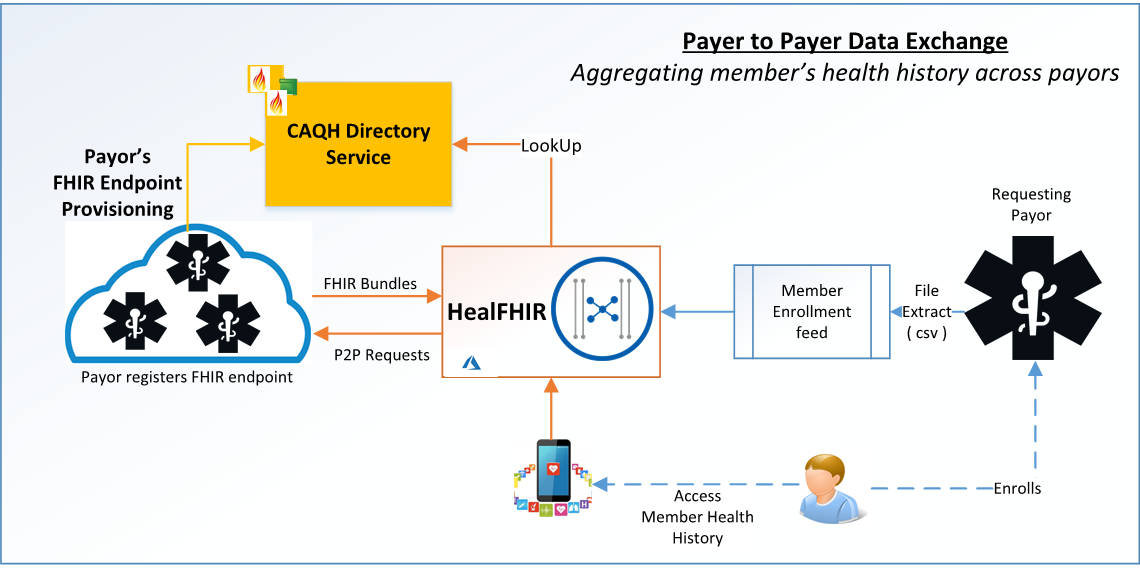
The HealFHIR admin portal takes in the member enrollment file, looks up the CAQH's directory service for appropriate payers' FHIR endpoint, and submits the member health history request. The returned FHIR bundle that is DaVinci's PDex implementation guide conformant is aggregated and uploaded to the HealFHIR server. The member's health history data aggregated from various payers is then made available to members via Patient Access API. For a more detailed look into how HealFHIR can help your organization, click the button below.
Sagitec’s HealFHIR is an infrastructure platform that keeps up with the changes to the FHIR specifications and CMS updates. It will also constantly test, validate, and enhance the list of payer FHIR endpoints.
For more information on HealFHIR integration with CAQH directory service, please contact:
You May Also Like
These Related Stories

Resources for Payers in the CMS InterOp and Patient Access API Journey

How to Choose the Best Pension Software Solution for your Organization




No Comments Yet
Let us know what you think